Neurotoxicity is a leading cause of pharmaceutical compound attrition. Drug-induced seizures can deprive the brain of oxygen resulting in brain injury and an increased incidence of mortality. These seizures are the result of excessive and synchronous firing of cortical neurons in the brain. Microelectrode array assays have emerged as a promising tool to predict seizure risk by measuring drug-induced changes to the spontaneous firing activity of neural networks in vitro. In this webinar, Dr. Benjamin Bader (NeuroProof) discusses how artificial intelligence-based machine-learning can be applied to these neural MEA datasets to improve the prediction of seizure risk.
Transcript of webinar:
Thank you for joining us on today's coffee break webinar, today's topic is using artificial intelligence to predict drug induced seizures in the brain. Neurotoxicity is a leading cause of pharmaceutical compound attrition, drug induced seizures can deprive the brain of oxygen resulting in brain injury and an increased incidence of mortality. These seizures are the result of excessive and synchronous firing of cortical neurons in the brain. Ion channel and receptor activity assays can be used to predict the seizurogenic potential of compounds in vitro however since these tests are often focused on a single target they can fail to detect neurotoxic compounds which rely on actions at a combination of targets. Seizurogenic compounds can also be identified later on in drug discovery by observing convulsive activity in rodents or dogs. Nevertheless it is possible that lower exposures of these same compounds may produce focal seizures, which are not observable as convulsions in the animal.
Neural microelectrode array assays can identify concentrations of a drug that produce increased neuronal firing that may be indicative of local seizures, but are not reported as a convulsion in vivo. Consequently a neural MEA assay could afford a more accurate prediction of seizurogenic compounds.
The new tox initiative is a public-private collaboration with the aim of characterizing the productivity of seizure genetic activity using MEA technology. Today's presenter Dr. Benjamin Bader brings more than 13 years of experience in neurobiology and stem-cell research, assay development and project management. He is a business director for customer projects and has led the molecular biology and assay development group at NeuroProof since 2010. Earlier in his career Dr. Bader obtained a master's of science and PhD in neurobiology and stem cell biology, and obtained international experience in the U.K. and Sweden. He will discuss how measuring drug induced changes to the spontaneous firing activity of mouse neural cells in MEA assays, help detect potentially harmful neurological side effects of compounds that were previously deemed safe.
Thank You, Melissa, for this kind introduction, as mentioned I will focus today on how to use MEA based assays to predict seizure liability in vitro.
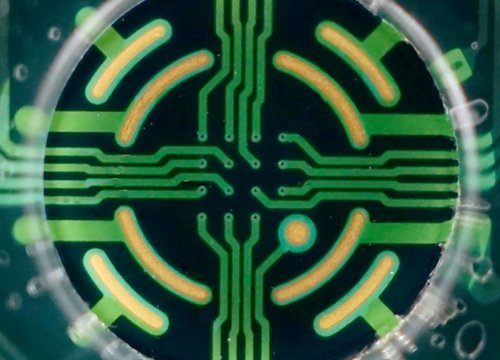
I want to start with a problem we all focus on in drug discovery, namely the safety aspect of seizure liability. As we know, and has been described in the literature, there are many drugs clinically used, which are associated with side effects such as convulsions or seizures, and there's a big need to develop new in vitro assays to avoid this in new drug candidates, and worldwide there are different organizations, listed here on the right hand side are some examples of them, which are developing new approaches and evaluating whether we can use the in vitro MEA readout for safety aspect evaluation. And we had NeuroProof also tackle that question of seizure liability prediction assays. After having developed this technological platform for more than 20 years and serving as a CRO partner for neuropharmacology and neurotoxin nutrition for more than 10 years now, we have developed a proprietary data analysis platform ,which is enhanced by artificial intelligence methods. They were having established assays and disease modeling following industry standards all using MEA readouts with neuronal cultures, which are spontaneously active, which then are described a hundreds of parameters which is then used for AI base similarity analysis and classification tools. We use the Axion Biosystems Maestro station and multi-well MEAs to record the spontaneous activity of embryonic mouse brain tissue cultures, or human iPS derived cultures and as you see in this heat map in the top right corner, or the life activity welds pie raster plot video in the bottom left corner, there are synchronized activities measurable, and these activities are then described by single spike raster plots per electrode, and then as a wells per spike raster plot for the complete number of electrodes. Now this activity pattern which is here, in this case synchronized can be changed by adding drugs, either inhibitory compounds or excitatory compounds. Another question is how we can describe this phenotypic change. We had NeuroProof compute hundreds of parameters and routinely use 200 of them to phenotypically describe effects of drugs or changes in the system, and these parameters includes general activity like spike and burst rate, but also oscillations, burst structure parameter, and more importantly also the synchronicity and connectivity readout all of those parameters, reflect the functional phenotype, and we call that fingerprint of a compound or a cell culture.
The cell culture we have been using for many years is the mouse embryonic brain region specific culture including cortex, hippocampus, ventral brain, spinal cord, etc, these cells are dissociated and replated on MEAs and then they mature over about four weeks into robust spontaneously active neural networks. This MEA technology allows compound screening either acutely or repeatedly.
Routinely, we use this cumulative addition of drug testings, starting with native activity for sixty to ninety minutes recording, and then applying accumulative increasing concentration of compounds. One example you see on this slide is methaqualone GABA receptor modulator, which is concentration dependently decreasing the activity, but this spike rate plot you see on the top, it's not the only parameter which is qualified as has been introduced, we have a heat map projection here developed which is showing 60 parameters of four categories reflecting the whole compound phenotype and that is very compound specific. And this compound specific fingerprint can then be compared with other compounds within the similarity analysis. The different fingerprints can now be compared by machine learning or classification approaches. As you see here, two examples of two GABA receptor modulators, from the heatmap alone it becomes evident that they are different in terms of their functional phenotype, but machine learning and classification allows assessing all of those parameters, to mode of action independently see, how functionally phenotypically similar or different they are. Further this allows the profiling against marketed drugs for repurposing actions, to evaluate off target effects, as well as toxicity prediction. As mentioned before there are several drugs associated with side effects such as convulsions or seizure in men, and the question is now, whether we can use the MEA readout to predict seizure-like effects in novel drug candidates.
One of those tool compounds usually applied in these prediction assays, is Picrotoxin which has a GABA receptor blocker and inducing seizures, and which is showing a hyperexcited state in this MEA readout, if you focus on spine grade only. Further it also induces these ictal-like events. The question is now whether we can use this multivariate analysis, to assess the seizure liability beyond this hyperexcitation, which is a hallmark of seizure but it is not predictive enough.
To calibrate a seizure essay we use 7 reference compounds which are known to induce seizure labeled in red, and which are non-seizurogenic labeled in green, all of them have in common that they are excitatory in the MEA readout to not compare excitatory with inhibitory compounds. Now using this multi parameter trick approach we show that all of them are excitatory, but they are very different if it comes to the complete fingerprint. There are several parameters where the three groups are significantly different from each other, and using machine learning and classification, we show that those two groups actually in a mode of action independent way are separated. In this separation, is now used to classify unknown compounds to see how predictive the assay is. We use this classifier now to predict whether some tool compounds, positive and negative compounds, are predicted correctly. On the left hand side you see known seizure-free compounds in a concentration response profile, showing here this spike rate, the table shows the seizure risk and percent using this classifier as introduced before, so all of those three seizure free compounds are safe. Whereas, the positive compounds increase the seizure liability and risk in a concentration dependent manner. Using the same approach we have evaluated different clinical compounds from our database and those associated with seizure actually show a transition from safe to seizure risk within their therapeutically relevant concentration labeled in blue. This can be linked with the seizure risk in men, and we performed the first trial to see whether there's a correlation of our in vitro prediction percentages, and the cases in men, and the table at the bottom shows that there is indeed a correlation. We had one false negative which is donepezil, but we should keep in mind that seizures are also symptoms in dementia, so that means that that can be the reason for this false negative, although at higher concentration the classifier predicts correctly that there might be a seizure risk associated with donepezil. As well summarizing the compounds we have tested so far shows that most of them are correctly classified as you see in the two right columns so the seizurogenic compounds have been predicted by our mouse in vitro assay and the non seizure compounds also have been correctly classified. We also used this approach to predict seizure liability in human iPS derived neurons, but for the sake of time I will not present that today. And so please stay tuned for some updates in the upcoming conferences. In summary I've shown you that our AI-based seizure prediction assay, is a readout which meets the need for predictive phenotypic in vitro assays, and the AI base machine learning allows the predicting of seizure risk at relevant concentration ranges both in mouse and human neurons. And, thereby it also meets the support of the 3r concept by replacing and reducing animals and use. And last but not least many thanks to you for interest and time today and I'm happy to take any questions by email.
And that is a conclusion for today's coffee break webinar, if you have any questions you would like to ask regarding the research presented, or if you are interested in presenting your own research with microelectrode array technology please forward them to coffeebreak@axionbio.com.
For questions submitted for Dr. Bader he will be in touch with you shortly.
Thank you for joining us on today's coffee break webinar, and we look forward to seeing you again!