“Man on Fire” syndrome, also known as Inherited Erythromelalgia (IEM), is a chronic pain syndrome characterized by burning pain in the hands and feet. The chronic pain of most patients with IEM cannot be relieved by common pain killers making this disease a major unmet medical need. In this webinar, Dr. Yang Yang (Purdue University) discusses advances in the treatment of IEM using a pharmacogenomic approach. The drug responsiveness of different genetic mutations associated with IEM were probed in an in vitro Maestro MEA assay, with the results helping to predict the effective treatment of these IEM patients in the clinic.
Transcript of Curing the Pain of Burning Man
Thank you for joining us on today's Coffee Creak Webinar. Today's topic is Curing the Pain of the Burning Man, targeting the NAV1.7 sodium channel.
Pain is a normal sensation that alerts us to possible injury when you cut your finger or pull a muscle pain. It is your body's way of telling you something is wrong. Once the injury heals you stop hurting. Chronic pain is different, your body keeps hurting weeks, months, or even years after the injury.
Doctors often define chronic pain as any pain that lasts for three to six months or more. Effective and safe pain management is a major unmet medical need. More than 100 million Americans suffer from chronic pain of varying degrees. The lack of effective but non-addictive painkillers partially contributes to the national substance abuse crisis. Potent analgesics including opiates are often addictive, others may be associated with poor tolerability resulting in sub-optimal pain control for many indications. Developing next-generation pain killers has enormous value.
Today Dr. Yang Yang will discuss advances in the treatment of an inherited chronic pain syndrome called Inherited Erythromelalgia (IEM) also known as 'Man on Fire' syndrome. By modeling pain in vitro in a microelectrode array assay, it's possible to predict the drug responsiveness of patients suffering from severe pain.
Dr. Yang obtained a PhD from Georgia State University and did post-doctoral training at Yale University School of Medicine. Dr. Yang is currently an assistant professor of Purdue University College of Pharmacy in the Department of Medicinal Chemistry and Molecular Pharmacology, also affiliated with the Purdue Institute for Integrative Neuroscience. His current research focuses on channelopathies of the nervous system including; pain, neuropathy, epilepsy, and autism. The WHI lab aims to understand how dysfunctions of ion channels contribute to these neurological diseases and to develop novel pharmacogenomic approaches targeting ion channels for disease intervention.
Thank you Melissa for a kind introduction, today I will be talking about a disease called Inherited Erythromelalgia (IEM) also known as "Man on Fire" syndrome. This is a very severe pain syndrome caused by mutations in a sodium channel called Nav1.7. I'm going to talk about how we use a pharmacogenomic approach to study the drug responsiveness of channel mutations and then translate our research to treat the patients with this disease.
Nav 1.7 channel has been regarded as the pain channel as this channel is directly involved in many different human pain syndromes.
On the left you can see a girl featured in the New York time magazine, she cannot feel any pain since her birth and can put her hand into boiling water without feeling anything, and then hurt herself.It is later found out that she has a loss of function mutation in her SCN9A gene since her body does not have a functional Nav 1.7 channel.
On the right, there are other patients who have very severe pain syndrome called Inherited Erythromelalgia (IEM), also known as Men on Fire Syndrome. Their pain is often triggered by milder ones. Duing each pain attack patients have burning pain sensation in their hands and feet and it turns out that these patients have super active Nav 1.7 channel caused by gain-of-function mutation in their SCN9A gene. More importantly, most patients with Inherited Erythromelalgia (IEM) are resistant to pharmacotherapy thus their pain cannot be relieved by common pain killers. Making this disease a major mathematical need.
Indeed we and colleagues have identified more than two dozen Nav 1.7 mutations that can cause IEM. As shown in the upper panel NAV 1.7 is a transmembrane protein having four domains. Each domain has six transmembrane helices the thoughts with number are different mutations finding patients who are suffering from pain syndromes, and you can see there are lots of them. It is noted that for these patients one size fits all pain medication does not work, therefore one of our major research goals says is to figure out how to use a precision medicine approach to treat these patients based on their genetic background.
As we mentioned most patients with IEM and Nav 1.7 mutations do not respond to any available pain medications. However, there are exceptions to most rules, so trial-and-error in the clinic, it has found that patients with one particular mutation V400M, responded to a drug called Carbamazepine.
Using patch-clamp analysis we found that Carbamazepine a novel mechanism of action on a mutiny channel by shifting the channel activation. Making the super active mutiny channel harder to open and acting more like a wild-type channel. The drug responsiveness of V400M was encouraging and motivated us to identify additional mutations that might be drug responsive. As often time structure determines function, we construct a human Nav 1.7 3D structure model to locate IEM mutations. Using this approach we identified another mutation which is S241T that is located very close to V400M. Indeed S241T and a V400M is 159 amino acids away in linear sequence their distance is only about a 3x chomp in a 3D structure. The proximity between these two mutations has hinted that they may affect the drug action of CBZ in a similar manner.
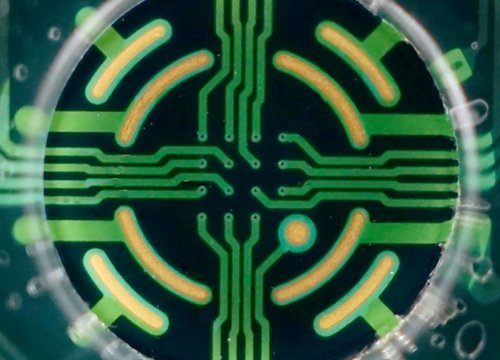
Structure modeling as well as many other assays we developed, but will not be covered in this talk helped us identify the new mutations that might be drug responsive. To further study the functional consequence of these mutations in intact pain sensing neurons and test the drug responsiveness of these neurons, we use the microelectrode array MEA system for our research. The MEA system is useful to us because it is an extracellular recording system that can monitor the action potential firing of neurons in their normal culture media.
The relatively high throughput nature of MEA can also help us to test many mutations with many different drugs at the same time. Additionally Inherited Erythromelalgia (IEM) this disease is triggered by warmth, MEA can also allow us to study the temperature effect of these neurons in aposition manner.
Using this MEA system we perform experiments to address our main question: can we really develop a precision medicine approach to guide the drug selection for IEM patients based on their genetic background? And here are the data we got, as you can see we use 33, 37 and 40 as the three temperatures for our study. And 33 represents the skin temperature, so 37 is the core body temperature, and 40 represents mild warmth. Each dot represents a neuron and their firing frequency is color-coded, you can see yellow and red means they are a high firing frequency, whereas blue-black means they're a low firing frequency. In the upper panel, we can see that in neurons expressing a Nav 1.7 - S241T mutation fire significantly more action potentials and the temperatures can drastically increase the firing of these neurons. Moreover, in the lower panel when we treated neurons with carbamazepine, the firing frequency, as well as the number of active neurons, was greatly reduced and we found that this difference a statistically significant.
On the other hand when we study carbamazepine on neurons expressing white hub channel, we did not see such a major effect of carbamazepine. Moreover, when we perform a similar recording of our different mutation F1449V we find that carbamazepine does not have a major effect on these neurons. Taking all this data together, demonstrated that the effect of carbamazepine is mutinous specific, suggesting a personalized treatment of this drug. All the data I described so far suggested that there is a new mutation, S241T may respond to carbamazepine.
Then the next bigger question is whether our products can be translated into the clinic and treated these patients. After nationwide search, we identify the two IEM patient's mothers and a son carrying S241T mutation who consented to participate in the study, and we carefully design a randomized placebo controlled,
double-blind crossover clinical trial for these two patients. The patient was given either placebo or carbamazepine for six weeks and then after two weeks wash out period, will cross over for another six weeks. Multiple parameters were recorded in patient's pain diary during the whole process. Functional MRI of the brain of these two patients was also performed during the trial to have a more objective measurement of the drug effect. Our clinical study generated very positive results as we can see from here.
Three major parameters, pain duration, absolute duration, and awakenings because of pain was very much reduced in carbamazepine treatment compared to the placebo treatment. Moreover, our functional MRI data showed that carbamazepine was able to switch the brain activity of these patients from chronic pain state to a cure the pain state, further demonstrating in a more objective manner that carbamazepine has a beneficial effect on patients caring S241T mutation.
I want to use this Burning Man image painted by one of our patients to end this story. This pain syndrome is very severe and very hard to treat. We hope through our research we can develop a new approach guided by genomic analysis and a functional profiling to provide a new way to extinguish the fire of the Burning Man and transformed pain treatment from trial and error to precision medicine in the near future.
Finally I want to acknowledge the people who helped with these studies, especially Dr. Steve Waxman and Dr. Sulayman Dib-Hajj, it is really a team effort to move this research from bench to bedside.
Thank you all for listening and that is the conclusion for today's coffee break webinar.
If you have any questions you would like to ask regarding the research presented or if you are interested in presenting your own research with microelectrode array technology,
please forward them to coffeebreak@axionbio.com
For questions submitted for Dr. Yang, he will be in touch with you shortly thank you for joining in on today's coffee break webinar and we look forward to seeing you again!